How CliniSearch works
CliniSearch lets clinicians ask clinical questions and get concise, cited answers from UK guidelines in seconds.
Search across NICE and specialty guidance in one place. Answers show the exact recommendation, source guideline, section, and version date — so you can verify and trust what you're seeing without opening PDFs.
Find the relevant section fast - with source proof
Clinical guidance is rarely wrong - it is just hard to locate quickly. CliniSearch lets clinicians ask questions in plain language and takes them straight to the most relevant section of the underlying guideline, without manual PDF hunting.
Every answer is anchored to its original source. You can see which organisation published the guidance, where the recommendation appears, and jump back to the exact section to verify the wording and context.
The result is faster orientation, fewer missed nuances, and a safer way to work when time is tight.
Three steps to a cited answer
CliniSearch is tuned for how clinicians actually ask questions.
Ask your question
Natural-language queries work: “When to refer CKD?”, “Anti-D in miscarriage?”, “LMWH duration after hip replacement?”
We search multiple guidelines
Queries NICE, RCOG, BSG, UKKA and more—matching both wording and meaning across structured guideline content.
You get a concise answer
Short summaries plus direct links to the source paragraphs and tables. Always see where the recommendation comes from.
What you get: answer + source proof
Clinisearch helps you find the relevant recommendation fast, with clear citations and a direct line back to the original guideline wording.
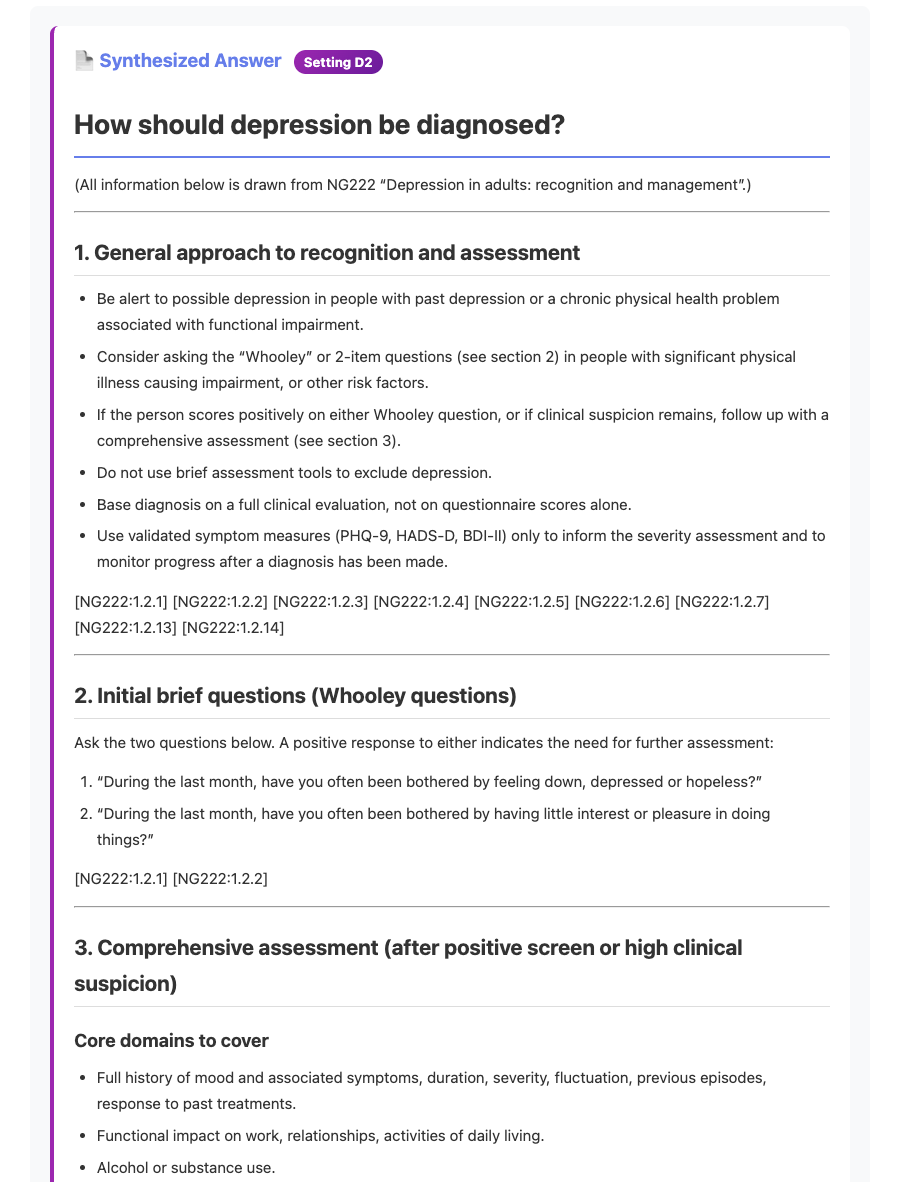
Example answer (what the user sees)
A short, readable answer with citations. This is the result view.
View verbatim NG222 excerpt (text)
Synthesized Answer Setting D2
How should depression be diagnosed?
(All information below is drawn from NG222 "Depression in adults: recognition and management".)
1. General approach to recognition and assessment
- Be alert to possible depression in people with past depression or a chronic physical health problem associated with functional impairment.
- Consider asking the "Whooley" or 2-item questions (see section 2) in people with significant physical illness causing impairment, or other risk factors.
- If the person scores positively on either Whooley question, or if clinical suspicion remains, follow up with a comprehensive assessment (see section 3).
- Do not use brief assessment tools to exclude depression.
- Base diagnosis on a full clinical evaluation, not on questionnaire scores alone.
- Use validated symptom measures (PHQ-9, HADS-D, BDI-II) only to inform the severity assessment and to monitor progress after a diagnosis has been made.
2. Initial brief questions (Whooley questions)
Ask the two questions below. A positive response to either indicates the need for further assessment:
"During the last month, have you often been bothered by feeling down, depressed or hopeless?"
"During the last month, have you often been bothered by having little interest or pleasure in doing things?"
3. Comprehensive assessment (after positive screen or high clinical suspicion)
Core domains to cover
- Full history of mood and associated symptoms, duration, severity, fluctuation, previous episodes, response to past treatments.
- Functional impact on work, relationships, activities of daily living.
- Alcohol or substance use.
- Co-existing physical health problems or medications that may contribute.
- Psychosocial stressors and social support.
- Risk of suicide or self-harm.
- Personal and family psychiatric history.
- Patient preferences and priorities for treatment.
Special populations
- People with a chronic physical health problem: integrate assessment with management of that condition [NG222:1.2.13].
- People with a diagnosis of personality disorder: follow recommendations in NG222 section 1.11 [NG222:1.11.3].
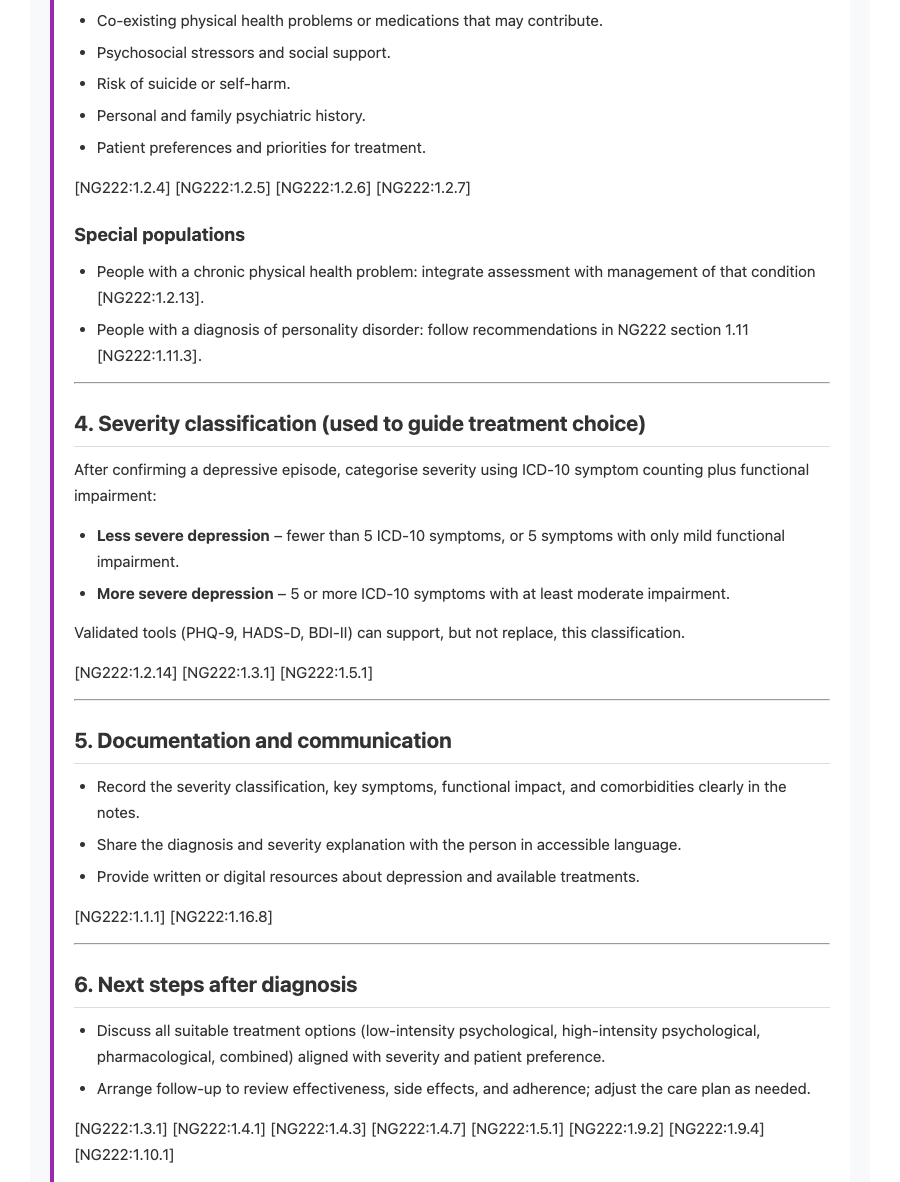
4. Severity classification (used to guide treatment choice)
After confirming a depressive episode, categorise severity using ICD-10 symptom counting plus functional impairment:
- Less severe depression - fewer than 5 ICD-10 symptoms, or 5 symptoms with only mild functional impairment.
- More severe depression - 5 or more ICD-10 symptoms with at least moderate impairment.
Validated tools (PHQ-9, HADS-D, BDI-II) can support, but not replace, this classification.
5. Documentation and communication
- Record the severity classification, key symptoms, functional impact, and comorbidities clearly in the notes.
- Share the diagnosis and severity explanation with the person in accessible language.
- Provide written or digital resources about depression and available treatments.
6. Next steps after diagnosis
- Discuss all suitable treatment options (low-intensity psychological, high-intensity psychological, pharmacological, combined) aligned with severity and patient preference.
- Arrange follow-up to review effectiveness, side effects, and adherence; adjust the care plan as needed.
Source guidance (verbatim, with pinpoint refs)
Every result is anchored to the original guideline text. Here’s an example excerpt (NICE NG222) showing severity classification, documentation, and next steps after diagnosis.
View guideline excerpt screenshots (NICE NG222)
Safety and governance built-in
Versioned sources, audit options, and proxy controls keep answers accountable.
Citations & versions
Every answer cites UK sources and tracks publication dates so you know which version you’re seeing.
Audit & identity
Enterprise logging captures query, user, IP, user agent, and correlation IDs; proxy injects user identity for accountability.
Controls that fit NHS
Request validation, rate limits, and analytics exports for Trust deployments. SSO, API, and intranet options available.
What happens after you hit search
Behind the scenes, CliniSearch runs a predictable pipeline that keeps answers fast, cited, and auditable.
Retrieval tuned for clinical intent
We normalise your query, map it to guideline concepts, and search structured content across NICE, RCOG, BSG, UKKA, BOA and more. Specialty filters keep results on-topic.
Responses are generated from guideline paragraphs—never unsupported hallucinations—with links to the original source so you can verify wording instantly.
Provenance stays attached
We keep the source guideline, publication date, and section reference with every answer. If a guideline updates, we refresh the embeddings and clearly mark the new version.
Enterprise deployments capture who asked the question, when, and which guideline paragraph informed the response—ready for CQC, QI, or clinical safety reviews.
Performance and coverage
Designed for the realities of clinic time and the breadth of UK guidance.
Fast by default
Heavily cached common queries, pre-processed guideline sections, and tight latency budgets keep responses under clinic pace. If something is slow, we return the citation links first so you can keep moving.
Broad UK coverage
NICE (NG/CG/QS), RCOG, BSG, UKKA, BOA, SIGN, and other UK specialty bodies are indexed with population tags so paediatric, pregnancy, or frailty nuances stay intact.
Works with your stack
Use the web app immediately, then add SSO, embed components, or API calls when you’re ready. The proxy normalises requests, enforces rate limits, and logs activity without slowing clinicians down.
